ABOUT STROKE
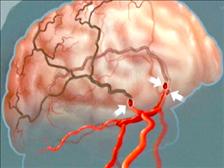
Stroke is the third leading cause of death in the United States and the leading cause of serious, long-term disability. It is a type of cerebral vascular disease in the brain that affects the arteries and blood vessels leading to and inside the brain.
A stroke occurs when a blood vessel that carries oxygen and nutrients to the brain is either blocked by a clot or bursts and causes bleeding. When that happens, part of the brain tissue cannot get the blood and oxygen it needs, so it starts to die. When part of the brain dies from lack of blood flow, the part of the body it controls is affected. Strokes can cause paralysis, affect language and vision and cause many other problems.
Hemorrhaging Stroke is caused by a rupture in a blood vessel near or in the brain. This rupture can stop the oxygen supply from reaching the surrounding areas of the brain. Usually symptoms are sudden and tend to affect younger people.
Ischemic Stroke
An Ischemic Stroke is a condition that affects the brain and the blood vessels supplying it. This happens when blood flow to a part of the brain suddenly decreases or stops. Blood carries oxygen and other nutrients to parts of the brain. When oxygen cannot get to the brain, brain cells may become damaged or even die. An ischemic stroke may begin suddenly and develop quickly. It can cause death of brain tissue within minutes to hours. Body functions such as walking or talking, are controlled by certain areas of your brain. An ischemic stroke can cause body functions controlled by areas of the brain to be lost.
What causes and ischemic stroke? An ischemic stroke may be caused by any of the following:
· A piece of fatty plaque formed in a blood vessel may break away and go to the brain. When this plaque blocks an artery (blood vessel), it causes an embolic stroke.
· A thrombus (blood clot) formed in an artery that supplies blood to the brain may cause a thrombotic stoke.
· A lacunar stroke happens when small blood vessels deeper inside your brain get blocked.
· In some cases, the cause of an ischemic stroke is not known.
| RISK FACTORS I CAN CHANGE OR CONTROL |
RISK FACTORS I CAN CHANGE OR CONTROL |
HIGH BLOOD PRESSURE
Diabetes
Tobacco use
Carotid or other artery disease
Heart disease (Atria fibrillation, Coronary Artery Disease)
Obesity
Physical inactivity
High cholesterol
A history of TIAs: Warning strokes
Excessive alcohol
Blood disorders that result in high red blood cell count |
Increasing age: people of all ages, including children, have strokes. But the older you are, the greater your risk for stroke
Heredity (family history): Your stroke risk is greater if a parent, grandparent, sister or brother has had a stroke
Race: African-Americans have a much higher risk of death from a stroke than Caucasians do, due to higher rates of high blood pressure, diabetes and obesity.
History of Stroke or Heart Attack: Someone who has had a stroke or hear attack is at higher risk of having a stroke |
TO REDUCE MY RISK OF STROKE, I WILL:
Stop smoking!
Lose weight!
Eat healthy foods!
Get Active!
Avoid excessive alcohol consumption! |
Have regular checkups to identify major risk factors.
Keep my blood pressure under control with lifestyle changes and/or medication
Keep my cholesterol under control with life-style changes and/or medication |
TREATMENT FOR STROKE
Acute Treatment:
Tissue Plasminogen Activator (TPA) is an FDA-approved, clot-busting drug. It must be administered within three hours from the onset of symptoms. Unfortunately, delays mean that only 3% to 5% of individuals who suffer a stroke reach the hospital in time t be considered for this treatment.
Preventive Treatment:
Antiplatelet agents such as aspirin, clopidogrel (Plavix), aspirin combined with extended release dypyridamole (Aggrenox) and anticoagulants such as warfarin (Coumadin) interfere with the blood’s ability to clot and can play an important role in preventing stroke.
Thrombolytics – This medication is used when a stroke is caused by clot in the blood vessel. Thromboyltic breaks apart clots and restores blood flow.
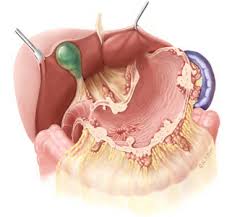
Carotid endoarterectomy is a procedure in which harmful plaque in the carotid artery is surgically removed.
Doctors can open blocked or narrowing arteries that are supplying blood to the brain by inserting a balloon angioplasty and/or implantable steel mesh tubes called stents.
Tell your doctor if:
· Your urine turns pink or red
· Your stools turn red, dark brown or black
· You bled more than normal when you have your period
· Your gums bleed
· You have a very bad headache or stomach pain that doesn’t go away
· You get sick or feel weak, faint or dizzy
· You think you’re pregnant
· You often find bruises or blood blisters
· You have an accident of any kind
How can an ischemic stroke be prevented?
· Do not smoke or drink too much alcohol. Smoking may harden blood vessels and cause conditions leading to ischemic stroke. Alcohol is found in beer, wine, liquor, like vodka or whiskey, and other adult drinks. Drinking too much too often can increase your risk of a stroke.
· Exercise regularly and stay at a health weight.
· If you have atrial fibrillation (an irregular or fast heartbeat), take antithrombotic medicine as ordered by your caregiver. You may also need this medicine if you had a heart attack.
· Keep your blood cholesterol level in a normal range. Eat foods low in fat to help prevent plaque from growing n your blood vessels. If you have high blood cholesterol levels, talk to your caregiver about ways to lower it.
· Manage your blood sugar level if you have diabetes. You may be told to change the way you eat to control your blood sugar. Ask your caregiver what your blood sugar levels should stay at.
· Take your blood pressure medicine as ordered, and check your blood pressure often. Ask your caregiver for more information about checking your blood pressure.
DIAGNOSTIC TESTS FOR STROKE
Diagnostic tests can usually outline the injured brain area by examining how the brain looks, works and gets its blood supply. The majority of these tests are safe and painless and non-invasive.
· Computed tomography (CT) scans create a picture of the brain using x-rays. The test results offer important information about the cause of the stroke, the location of the stroke and the extent of the brain injury. Thus, CT scans are usually one of the first tests given to patients suspected of stroke.
· Magnetic Resonance Imaging (MRI) creates an image of the brain using a large magnetic field. Similar to the CT scan, the test results show the location and extent of brain injury. MRI images are often used to diagnose small, deep injuries, as they are sharper and more detailed than CT scans.
· Angiography (arteriorgraphy or arteriogram) are special dyes injected into the blood vessels (through a catheter) and an x-ray is taken. This test evaluates the size and location of blockages.
· Echocardiogram is a type of ultrasound using sound waves to show pictures of the size and shape of your heart. It also looks at how your heart moves when it is beating.
· Doppler testing is when a probe is placed over the suspected artery, usually in the neck or at the base of the skull, and the amount of blood flow is determined using ultrasound technology.
Frequently Asked Questions About Stroke
What are the risk factors for stroke?
There are many factors that increase the risk for stroke. High blood pressure, diabetes, heart disease, tobacco and drug use, obesity, inactivity and alcohol abuse are the most common risk factors associated with stroke.
What are the warning signs of stroke?
· Numbness and weakness of face, limbs and/or on one side of the body
· Confusion
· Slurred or inappropriate word usage
· Inability to speak, swallowing or understanding
· Lack of mental clarity
· Loss of balance and coordination
· Loss of vision in one eye or inability to see clearly
*If you experience any of the above, note the time of onset and call 911 immediately*
What is a “mini stroke” or TIA?
TIA also known as a “mini stroke” is a temporary stroke that produces stroke symptoms that only last for a short amount of time.
Can I drive after a stroke?
Driving after a stroke is not always the best decision. Before getting back into the drivers seat, you should contact your doctor and he/she will provide you with their professional opinion. It is also a very good idea to have your driving tested after a stroke to keep you and your family in safe hands.
Is it normal to feel tired after a stroke?
Yes, it is very common to feel tired after a stroke. Some people are affected more than others due to physical and emotional changes in their lifestyle.
How long will I have to stay at the hospital after a stroke?
Depending on the severity of the stroke, your doctors will evaluate your ability to care for yourself, and will send you home at the appropriate time.
How can I reduce the risk of another stroke?
The best way to reduce your risk of another stroke is to lead a healthy lifestyle. You can do this by maintaining proper nutrition, eliminating tobacco use, reducing alcohol intake, and paying close attention to your physicians’ recommendations.
Call 911 immediately if you experience any of these stroke warning signs:
· Sudden numbness or weakness of the face, arm or leg, especially on one side of the body.
· Sudden confusion.
· Trouble speaking or understanding
· Sudden trouble seeing in one or both eyes
· Sudden trouble seeing in one or both eyes
· Sudden trouble walking, dizziness, loss of balance or coordination
· Sudden severe headache with no known cause
......................................................................STROKE AND APHASIA...............................................................................
What is aphasia?
Aphasia is a language disorder that affects the ability to communicate. Aphasia is most often caused by stroke that affects the left part of the brain which controls language. People with aphasia are often frustrated and confused because they cannot say what they mean. The jumbled understanding and communication may improve with the proper rehabilitation.
Stroke survivors that are affected by Aphasia, remain mentally alert and can still have:
· Trouble speaking
· Trouble finding the right words to say
· Problems understanding others
· Inability to process long words and infrequently used words
· Trouble recognizing words
Different Types of Aphasia
Global aphasia: A person may completely be unable to speak, name objects, repeated phrases or follow commands
Broca’s aphasia: The person knows what they want to say, but can’t find the right words.
Wernicke’s apahsia: A person can barely comprehend what is being said or control what they are saying.What is Stroke Rehabilitation?
For many stroke patients, rehabilitation is a critical part of recovery. A patient may have difficulty functioning:
· Physically (unsteady gait, weakness or paralysis)
· Cognitively (confusion, memory and/or language problems)
· Emotionally (irritability, anxiety and/or depression)
The effects of a stroke may mean that one must change, relearn or redefine ones lives. Each patient is unique and rehabilitation is tailored to the individual’s specific needs. Successful rehabilitation depends on:
· How early rehabilitation begins
· The extent of the brain injury
· The patients attitude
· The expertise and dedication of the rehabilitation team
· The cooperation of family and friends
Who is the rehabilitation team?
A rehabilitation doctor (physiatrist), rehabilitation nurse, physical therapist, occupational therapist (OT), speech – language therapist, neuropsychologist, and recreation therapist.
When does rehabilitation begin?
Rehabilitation will begin when the doctor determines that the stroke patient is medically stable. Rehabilitation services are provided in many different places throughout the North Shore Long Island Jewish Health System.
Types of rehabilitation:
Acute care and rehabilitation hospitals
· Designed for individuals who need frequent physician monitoring and intensive daily and physical occupational therapies.
· Length of stay from 2-3 weeks
· Followed by sub-acute, outpatient or home based rehabilitation.
Sub-acute rehabilitation hospital
· Designed to provide continued rehabilitation therapies and skilled nursing care in an inpatient setting.
· Length of stay could range from 2-12 weeks

............................................................Stroke Caregivers....................................................................................
It is extremely important to have someone provide help for stroke survivors. A caregiver can be anyone willing to help provide the most care. A spouse, family member and friends are always great “care partners”.
Each caregiver’s responsibilities vary according to the needs of the stroke survivor. Some common responsibilities of care giving include:
- Physical help with personal care
- Transportation assistance
- Managing financial, legal and business affairs
- Ensure safety
- Meal preparation
- Providing comfort
- Housework
- Monitoring medications
- Rehabilitation assistance
- Emotional support
- Positive reinforcement
- Encouragement
Living at Home After Stroke
When is it time to go home?
Most stroke survivors are able to return home and resume many of their everyday activities. Your doctor may advise you to move to another facility that can help you meet your needs. It is important that the living place you choose is safe and supports your continued recovery. If you are ready to leave the hospital it may seem scary at first because things may have changed. Going home poses a few problems for people who have lingering effects.
There are four factors that you should consider before going home:
· Ability to care for yourself
· Ability to follow medical advise
· A caregiver (someone who is willing go help)
· Ability to move around and communicate
What changes do I need to make at home?
Safety and Accessibility. Living at home successfully depends on how safely and easily you can move throughout the house. Your home should be modified so you can be as independent as possible. A good idea for those who have lingering effects is to add adaptive equipment like grab bars, ramps, handrails or transfer benches ADDITIONAL RESOURCES
American Stroke Association
(A division of American Heart Association)
www.strokeassociation.org
1-800-4STROKE
National Stroke Association
www.stroke.org
1-800-STROKES
The Brain Attack Coalition
www.stroke-site.org
(301) 496-5751
Stroke Family
(speech recovery)
www.strokefamily.org
1-877-835-3157.
|
TRANSIENT ISCHEMIC ATTACK
GENERAL INFORMATION:
What is a transient ischemic attack? Transient ischemic attack is also called a TIA or a mini stroke. It may be a warning signal before a stroke occurs. A stroke is like a TIA but may cause permanent damage to the body. TIA happens when blood flow to the brain is decreased. When this happens, oxygen going to the brain is also decreased. This may lead to loss of certain body functions controlled by the part of the brain affected by the TIA. The effects of a TIA last for a few minutes to an hour. All effects are gone in less than 24 hours and do not cause permanent damage to the brain or body.
What causes a transient ischemic attack? High blood pressure or diabetes may make you more likely to have a TIA. Other causes may be high amounts of cholesterol (fat) in the blood or smoking.
What factors put me at a higher risk of having a transient ischemic attack? The following factors may put you at a higher risk of having a TIA:
· Atherosclerosis (hardening of the arteries) or fat deposits on the walls of an artery (blood vessel).
· Cigarette smoking, cocaine use, or drinking too much alcohol.
· Diabetes
· Heart disease, such as coronary artery disease.
· High blood cholesterol.
· High blood pressure.
· You or a close family member has had a stroke in the past.
What are the signs and symptoms of a transient ischemic attack? Signs and symptoms of a TIA depend on the brain affected. During a TIA, you may have numbness (loss of feeling), tingling, weakness, or paralysis (loss of movement). You may have trouble walking, swallowing, talking, or understanding. Your vision (sight) may be blurred or doubled. If you have one or more of these signs and symptoms, it is an emergency. Call 911 or 0 (operator) to activate the EMS (emergency medical service). Ask for an ambulance to get to the nearest hospital. Do not drive yourself.
How is a transient ischemic attack diagnosed? You may have any of the following tests to diagnose a TIA:
· CT Scan:
· This is also called a CAT scan. A special x-ray machine uses a computer to take pictures of your brain. It may be used to look at bones, muscles, brain tissue, and blood vessels.
· You may be given dye before the pictures are taken. The dye is usually given your IV. The dye may help your caregiver see the pictures better. People who are allergic to iodine or shellfish (lobster, crab, or shrimp) may be allergic to some dyes. Tell the caregiver if you are allergic to shell fish, or have allergies or medical conditions.
· MRI: This test is called magnetic resonance imaging. During the MRI, pictures are taken of your head. An MRI may be used to look at the brain, muscles, joints, bones, or blood vessels. You will need to lie still during a MRI. Never enter the MRI room with an oxygen tank, watch, or any other metal objects. This can cause serious injury. Tell your caregiver if you have any metal implants in your body.
How is a transient ischemic attack treated? You may need medicines to thin your blood, melt blood clots, or lower your blood pressure. Sometimes surgery is needed to remove a blockage from an artery.
What can I do to prevent a transient ischemic attack? To prevent a transient ischemic attack:
· Do not smoke. This will reduce your risk of a TIA and stroke.
· If you have atrial fibrillation (an irregular or fast heartbeat) or a recent heart attack, you may need antithrombotic medicine. Taking these medicines exactly as ordered may help prevent a TIA.
· Keep your blood cholesterol level in a normal range. If you have hyperlipidemia (high blood cholesterol), talk to your caregiver about ways to lower it.
· Monitor a control your blood sugar level if you have diabetes.
· Take your high blood pressure medicine regularly.
· Do not drink alcohol. Alcohol is found in beer, wine, liquor (such as vodka or whiskey), and other adult drinks. Talk to your caregiver if you drink alcohol.
· Exercise regularly, and be at healthy weight.
FACTS ABOUT SECONDHAND SMOKE
· Secondhand smoke is classified by the Environmental Protection agency as a known cause of lung cancer in humans (Group A Carcinogen). Same as Asbestos.
· Secondhand smoke contains more than 4,000 chemicals. Many of them are harmful to the body.
· Smoke-filled rooms can have up to six times the pollution of a crowded highway.
· Secondhand smoke is linked to lung, cervical, breast, and bladder cancer.
· Secondhand smoke is associated with 35,000 heart attacks each year in nonsmokers.
HOW DOES SECONDHAND SMOKE AFFECT CHILDREN?
· Children who live with a smoker inhale 102 packs of cigarettes by the age of 5!
· Infants and children whose parents smoke are seriously affected by exposure to secondhand smoke. Secondhand smoke puts them at higher risk to develop more colds and pneumonia-it also makes asthma worse.
· Children exposed to secondhand smoke are also more likely to have reduced lung function and symptoms of respiratory irritation like coughing, excess phlegm, and wheezing.
· Secondhand smoke can lead to middle ear infections.
TIPS TO MAKE YOUR ENVIRONMENT SMOKE-FREE
· Do not allow babysitters or others who work in your home to smoke in the house or near your children.
· Insist that your child’s school and/or day care program be smoke-free.
· Do not smoke or allow others to smoke in your care. Even if you are alone in the car.
· I t is not ok to smoke in the kitchen with the exhaust fan on or with the window open. It is not only the smoke in the air that is harmful but the particles that settle in the carpet, drapes and furniture that is linked to many serious health problems.
· If you do smoke, the best thing you can do is try to stop.
3 COMMON MYTHS ABOUT SECONDMAND SMOKE
Myth # 1
Secondhand Smoke doesn’t contain the same chemicals as tobacco smoke. Secondhand smoke contains all the same cancer-causing chemicals.
Myth #2
It’s my right to smoke where I want! Everyone has the right to a smoke free environment. Secondhand smoke causes 300,000 cases of pneumonia and bronchitis each year.
Myth #3
Secondhand smoke doesn’t really affect my children.
Babies of parents who smoke are twice as likely to die from Sudden Infant Syndrome. Children living with smokers, are much more likely to start smoking!
Stop Smoking Programs for Teenagers
MAYBE YOU NEED MORE REASONS TO CONSIDER QUITTING?
· Maybe you are tired of your parents as king/ begging you to quit.
· Maybe you are tired of hiding your smoking from parents, teachers, and coaches.
· Maybe you would like your hair, clothes and breath to smell clean and fresh.
· Maybe you would like to improve your ability to exercise and play sports.
· Maybe you are sick of wasting money on cigarettes.
BE AWARE OF THE RISKS ASSOCIATED WITH SMOKING
PREMATURES WRINKLES
BAD BREATHE
SEVERE ACNE
SEXUAL DYSFUNCTION
DIFFICULTY EXERCISING AND PLAYING SPORTS
TOOTH AND GUM DISEASE
SENSE OF TASTE AND SMELL IS DECREASED
MORE SUSCEPTIBLE TO COLDS AND BRONCHITIS AND ASTHMA
INCREASE IN HEART RATE AND BLOOD PRESSURE
HEART DISEASE AND STROKE
CANCER
STOMACH ULCERS
GETTING STARTED
· You become positively that you want to quit!
· Write down the reasons why you want to quit smoking.
· Set a target-quit date in the next 2 weeks. Don’t allow anything to interfere with that date.
· Identify obstacles to quitting. Make a plan overcome them.
· Make a list of people who can support your intentions to quit.
· Discard cigarettes, ashtrays and lighters.
YOU ARE ADDICTED TO NICOTINE IF…
· You become irritable and uncomfortable when you try to quit using tobacco.
· You have a strong urge to use it.
· You don’t feel normal in social situations without it.
· You continually increase the amount you use of it.
· You reach for a cigarette when you feel stressed.
· You’ve lied about using it!
CHEMICALS FOUND IN CIGARETTES
AMONIA-TOILET BOWL CLEANER
BUTANE-LIGHTER FLUID
CADIUM-BATTERIES
STEARIC ACID-CANDLE WAX
HEXAMINE-BARBECUE LIGHTER
ARSENIC-POISON
METHANE-SEWER GAS
CARBON MONOXIDE-CAR EXHAUST